Atrial Tachycardia
Overview
Atrial tachycardia (AT), by definition a type of supraventricular tachycardia (SVT), originates from a “focus” in either of the two top atrial chambers with a heart rate of > 100 beats per minute. Atrial tachycardia occurs when a portion of the atrial tissue speeds up and overtakes the normal sinus node as the pacemaker site of the heart. The symptoms of atrial tachycardia are similar to other SVTs, with palpitation, lightheadness, dizziness, shortness of breath, reduced exercise capacity, weakness, fatigue, chest discomfort, and sweating episodes. These symptoms are primarily due to loss of atrioventricular synchrony (when then atria and ventricles no longer contract in a tightly-coupled progression) or the development of rapid and/or irregular ventricular rates.
Mechanism and Causes
There is no definitive answer as to why AT occurs in some persons and not others. Atrial tachycardia is seen in patients both with and without structural heart disease. It can originate from virtually any “focus” or spot in the left or right atrium, with abnormal atrial tissue “firing”.
Figure 1. Animation of an atrial tachycardia with an atrial focus firing, typically faster than the sinus node, leading to a focal atrial tachycardia.
Diagnosis
Atrial tachycardia can be diagnosed by your physician via an electrocardiogram or an ambulatory monitoring device, i.e. Holter or Event monitor, specifically during an arrhythmia episode. Some episodes of AT are intermittent and not reliably present on a daily basis. In these situations, your physician may recommend a special ambulatory monitoring device that is patient-triggered, i.e. an Event monitor.
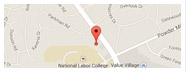
Atrial tachycardias have a predilection for origination from specific right atrial and left atrial anatomic structures. Your physician can use the 12-lead EKG performed in the office or hospital to help localize the site of origin based on the morphology of the p-wave (represents cardiac atrial activation). The width, height, and directionality of the p-wave holds a clue to its site of origin. In addition, patients may have multiple atrial tachycardias that fire at the same or different times.
Figure 2. Single-lead EKG strips of different p-wave morphologies (shown with arrows) during atrial tachycardia. The shape and directionality of the p-wave on the surface EKG (which represents atrial contraction) provide clues to the location of the atrial tachycardia focus.
Because Ambulatory monitoring devices, such as Holter monitors and Event monitors are only able to record one or two EKG leads, they provide less information regarding the electrical activation of the top atria. Not only does this limit the precise localization of the AT focus in the heart, but it also limits the discrimination of the arrhythmia and the making of a precise diagnosis. For patients who require an unequivocal diagnosis, or who are candidates for a “curative” catheter ablation procedure, an intracardiac electrophysiology study is the “gold standard” test to establish the diagnosis (see below).
Prognosis
Atrial tachycardia, as an isolated rhythm disturbance, is not considered a life-threatening condition. Some patients are able to control their episodes with life-style modification. This includes avoidance of caffeinated beverages, alcohol, sleep-deprivation, stressful situations, and anxiety. Spontaneous resolution of symptomatic episodes is uncommon. Prolonged episodes (typically man months or years) of continuous atrial tachycardia can be problematic. Atrial tachycardia can cause irreversible changes to the atria, including negative remodeling with atrial enlargement and weakness (myopathy). In addition, prolonged episodes can make reversion and maintenance of normal sinus rhythm more difficult. Long-lasting atrial tachycardia with continuously rapid ventricular rates (heart rates typically greater than 100 beats per minute) may cause a tachycardia-induced cardiomyopathy (weakening of ventricular muscle and heart function) and symptoms of congestive heart failure. In recent years, the significance of AT in the initiation and perpetuation of atrial fibrillation has become apparent.
Therapy
Therapy for patients suffering from atrial tachycardia depends on the frequency and severity of symptoms. Your physician may decide to implement therapy with oral medications if you are having frequent episodes that affect your daily living. Therapy for AT has three components:
- Control of the ventricular rate (heart rate)
- Maintenance of sinus rhythm during asymptomatic periods (suppression of AT)
- Cardioversion to normal sinus rhythm during symptomatic AT episodes
This can be achieved with either:
- Medical management
- Curative catheter ablation
 Medications used to control the ventricular rate during AT episodes include b-blockers, calcium channel blockers, and less commonly digoxin. These medications can be administered orally on a routine outpatient basis, or via intravenous route if necessary in the emergency room. These medications may also have an influence on suppressing AT episodes, with a clear decrease in the frequency and severity of symptoms. Some patients may need a combination of medications from different classes. Patients may experience alleviation of symptoms either due to a reduced burden of AT episodes or from the slowing of the ventricular response (heart rate) with the use of b-blockers or calcium-channel blockers that delay electrical conduction through the AV node.
Medications used to control the ventricular rate during AT episodes include b-blockers, calcium channel blockers, and less commonly digoxin. These medications can be administered orally on a routine outpatient basis, or via intravenous route if necessary in the emergency room. These medications may also have an influence on suppressing AT episodes, with a clear decrease in the frequency and severity of symptoms. Some patients may need a combination of medications from different classes. Patients may experience alleviation of symptoms either due to a reduced burden of AT episodes or from the slowing of the ventricular response (heart rate) with the use of b-blockers or calcium-channel blockers that delay electrical conduction through the AV node.
Attempts to maintain sinus rhythm can be approached with antiarrhythmic drug therapy if the previously mentioned medications fail to alleviate symptoms. These pharmacologic therapies can act directly on the cardiac substrate by slowing electrical conduction in the heart and lengthening the time required for electrical recovery of heart tissue, therefore preventing these atrial “foci” from firing and perpetuating themselves. Many patients will ultimately require treatment with antiarrhythmic drugs for termination and suppression of their atrial tachycardia. Drug therapy for AT is a “trial and error” proposition; it is not possible to determine ahead of time which medication will work the best in a particular patient. Maintenance of sinus rhythm with complete suppression of AT may not always be possible with medications. Improvements in your quality of life must constantly be reevaluated in relation to the small risks, discomfort, and potential side effects associated with your prescribed treatment regimen. Antiarrhythmic medications are not without risk, as they can increase the incidence of other cardiac arrhythmias.
For those patients who elect to forgo medication either due to
- intolerable symptoms or side effects from their medications,
- recurrent symptoms and episodes despite medical therapy, or
- lack of desire to take daily medications for an extended period of time,
your physician may recommend you undergo an electrophysiology study (EPS) and possible “curative” catheter ablation. In brief, these procedures are performed in a special procedure room called an electrophysiology (EP) laboratory. The EP laboratory houses a table and an x-ray (fluoroscopy) machine that is suspended over the table. With the use of specialized electronic and computer equipment, in conjunction with the intracardiac electrode catheters (placed into the heart via the femoral veins), your heart rhythm specialist can map the origination of your extra beats and AT under fluoroscopic and electrical guidance with the goal of delivering radiofrequency energy to that site and eradicating the rhythm disturbance. Radiofrequency energy employed during the catheter ablation procedure heats the tissue enough to destroy the local heart cell function, but without physically cutting through the tissue. The long-term success rate does depend on the location of the AT, with a response of >85-90% common.





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office