Atrioventricular (AV) Block
A slow heart rate can be due to many causes, including the earlier described sick sinus syndrome (SSS). Another cause, atrioventricular block (AV block), is due to abnormally slowed electrical conduction of the sinus impulse through the AV node. The extreme variant of this can manifest as complete AV block, with no sinus impulses able to traverse a diseased AV node, and complete disconnection between the top (atria) and bottom (ventricular) chambers.
As described earlier, the sinus node, a structure in the high right atrium, depolarizes typically 60 to 100 times per minute sending an electrical impulse throughout both atria to the AV node. In brief, this leads to synchronized biatrial contraction before ventricular contraction forces blood out of the heart into the circulation. The AV node, a structure that sits in the middle of the heart, is normally the only electrical connection between the atria and the ventricles. The AV node serves as a traffic signal, controlling the rate of electrical impulses from the atria allowed to reach the ventricles, limiting the danger of 1 to 1 conduction of fast rhythms from the atrium to the ventricles.
AV block is a term to describe abnormal impulse conduction through the AV node. This can be manifest as slower than usual propagation through the AV nodal structure to the ventricles, or complete disconnection of the atrial electrical signals to the ventricles.
 Figure 1. Animation of the sinus node impulse propagating to and through a diseased AV node. In AV block, as depicted above, the electrical impulse is delayed for longer than usual in the AV node, and may at times fail to conduct further into the ventricles.
Figure 1. Animation of the sinus node impulse propagating to and through a diseased AV node. In AV block, as depicted above, the electrical impulse is delayed for longer than usual in the AV node, and may at times fail to conduct further into the ventricles.
More specifically, the types of heart block are:
- First-degree AV block: electrical impulses are slowed through the AV node, but there is still 1 to 1 conduction to the ventricles with delay. Rarely do patients exhibit symptoms from this condition, and it may be a normal finding in well-conditioned athletes reflecting a high vagal tone. Medications can also contribute to this finding. The classic EKG finding of this condition is a prolonged PR interval.
- Second-degree AV block Type I (also known as Mobitz Type I or AV Wenckebach): in this condition, there is progressive delay in conduction of each subsequent atrial impulse reaching the AV node, to the ventricles. Finally, an atrial impulse is blocked in the AV nodeand fails to conduct to the ventricles, leading to a skipped beat. The 12-lead EKGmanifestation of this condition is a progressive prolongation in the PR interval with a resultant p-wave not followed by a QRS. Mobitz Type I AV block can be normal during periods of high vagal tone, as with sleep. However, it can be symptomatic leading episodic dizziness and lightheadedness.
- Second-degree AV block Type 2 (also known as Mobitz Type II): in this condition, there does not appear to be a delay in AV nodal conduction on the surface EKG with a normal PR interval; however, there will be episodic atrial impulses that are blocked in the diseased AV node and do not conduct to the ventricles. This condition is less common than Mobitz Type I AV block and substantially more serious. It can herald progression to third-degree heart block (also known as complete AV or heart block). Your physician will need to examine you carefully to determine if a permanent pacemaker is necessary.
- Third-degree AV block (complete heart/AV block): in this condition, atrial impulses are completely blocked from reaching the ventricles, with electrical disconnection of the two chambers. There may be a secondary, yet slower-beating site in the ventricles that takes over the pacemaker function of the heart. This condition is dangerous as this backup pacemaker site is not reliable and complete loss of cardiac electrical activity with cardiac arrest could be imminent. A pacemaker is generally warranted in situations that are not secondary to other medical conditions that may resolve or improve (i.e., heart attack, medications, electrolyte disturbances); if there will be delay, a temporary transvenous pacemaker may be placed by your physician in the interim.
Symptoms
The symptoms of AV block are similar to sick sinus syndrome (SSS), and are a direct product of the resultant slow heart rates. These include palpitations, skipped-beats, dizziness, lightheadedness, syncope (loss of consciousness), fatigue and weakness, confusion, and even angina (chest pain). Any symptoms of syncope or chest pain require urgent medical evaluation.
Causes
AV block can be the result of normal wear and tear on the AV node that occurs with age. In addition, patients post-cardiac surgery, particularly valvular surgery, are at a high-risk of complete AV block necessitating permanent pacemaker implantation. Medications, particularly for hypertension, can exacerbate already slow conduction through a diseased AV node leading to symptomatic AV block. Acute coronary syndromes, i.e. heart attacks, can lead to transient versus permanent degrees of AV block. Patients undergoing alcohol septal ablation for hypertrophic cardiomyopathy are also at risk for developing complete heart block.
Treatment
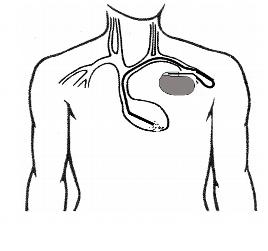 Patients with asymptomatic Type I or Mobitz Type I second-degree AV block require no further treatment. Patients with third-degree or complete heart block that does not resolve and that is not secondary to a transient condition, will require implantation of a permanent pacemaker. Those patients with either symptomatic Mobitz Type I second-degree AV block or Mobitz Type II second-degree AV block will need further referral to a cardiac specialist for possible implantation of a permanent pacemaker. This procedure is described in the pacemaker section, but in brief, it involves the creation of a pocket under the skin of the upper chest for the small electronic pacemaker device to be implanted.
Patients with asymptomatic Type I or Mobitz Type I second-degree AV block require no further treatment. Patients with third-degree or complete heart block that does not resolve and that is not secondary to a transient condition, will require implantation of a permanent pacemaker. Those patients with either symptomatic Mobitz Type I second-degree AV block or Mobitz Type II second-degree AV block will need further referral to a cardiac specialist for possible implantation of a permanent pacemaker. This procedure is described in the pacemaker section, but in brief, it involves the creation of a pocket under the skin of the upper chest for the small electronic pacemaker device to be implanted.
Electrical signals from the pacemaker are delivered to the heart via one or two implantable intracardiac leads inserted through the veins of the chest underneath the clavicle. The pacemaker’s electronic circuitry will monitor the heart rhythm and rate 24 hours a day, seven days a week. It will deliver an electrical impulse and pace the heart, only when the heart rate slows or there is a pause, thus eliminating symptomatic episodes of bradycardia (slow heart rate). In cases of complete heart block, the lower ventricles will be essentially paced 100% of the time.





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office