Permanent Pacemaker
What is a pacemaker?
A pacemaker is small battery-operated device, typically weighing about an ounce, that is packed full of electrical circuitry and a battery (the “generator”) with the sole function to monitor your own heart’s rhythm and electrically pace your heart if your own heartbeat becomes too slow. The pacemaker system consists of the pulse generator (typically referred to as the “pacemaker”) and one or two pacing leads, placed into the heart. There are over 3 million people worldwide with pacemakers, including not just adults, but children as well.

Figure 1. Image of a typical pacemaker generator along side a “key”. Note the relative size of the two objects.
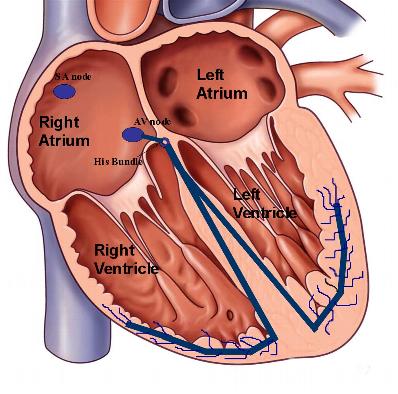
As discussed in the previous sections, your normal heart has its own pacemaker comprised of specialized conduction cells in the top right atrium, known as the sinus node. The sinus nodetypically fires at a rate of 60–90 times per minute. This electrical depolarization wave leads to the contraction of the upper atria with the signal traversing the AV node, located in the center of the heart in between the upper and lower chambers, to the ventricles with synchronized ventricular contraction. Any site of slow, or blocked, conduction along this specialized network of conducting tissue may lead to slow heart rhythms, or bradycardias, that necessitate placement of a permanent pacemaker system.
Figure 2. Schema of the normal conduction system of the heart.
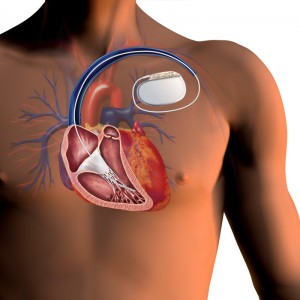
The pacemaker “generator” is typically slightly larger than a man’s wristwatch. A permanent, or artificial, pacemaker has connecting intracardiac leads that are positioned into the heart to allow for pacing the heart tissue directly. The pacemaker leads are essentially insulated wires that allow for the pacing electrical impulses to be conducted from the generator to the tip of the leads.
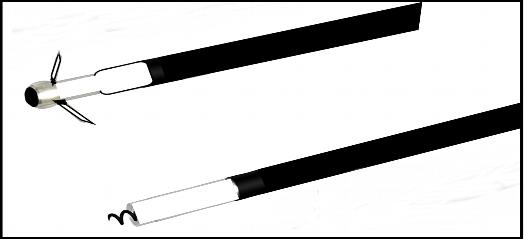
Figure 3. Specialized pacemaker leads have electrodes at their tips that allow them to sense the electrical activity in the heart. As well, they are able to deliver electrical current to pace the heart. The top lead is known as a passive fixation system, or “tines”, that capture themselves in the heart muscle tissue to maintain a long-term stable position. The bottom lead is a active fixation system that consists of a distal end with a screwing mechanism to allow it to maintain stability in the position that your physician implants.
The intracardiac pacemaker leads are implanted via the central chest veins and using fluoroscopic, or X-ray, guidance they are maneuvered into position into the right-sided heart chambers. Some intracardiac leads have distal, or end, screws that can be deployed at the time of implantation to maintain the lead position. The opposite-end of the intracardiac lead is then screwed into the generator. Once implanted, these leads can sense your heart’s own electrical signals and if too slow, pace accordingly. A small electrical current created by the pacemaker generator flows from the generator through the insulated intracardiac leads to the interface between the lead tip and the heart muscle tissue. The pacemaker is then programmed to pace your heart if it falls below a lower programmable rate, as determined by your physician.
Figure 4. Illustration of a typical pacemaker system. The pacemaker generator is usually placed in the left chest, just underneath the skin. The pacemaker leads are placed into the heart via the central veins in the chest and screwed into the “header” of the pacemaker generator.
There are two types of pacemaker systems. They differ only in the number of intracardiac leads positioned into the heart. A single-chamber pacemaker refers to a device with a single lead, typically a right-ventricular pacing lead; whereas a dual-chamber pacemaker includes a second lead, hence, both a right atrial and right ventricular lead. For those patients with a history of sick-sinus syndrome or bradycardia originating from the atria, they typically benefit from implantation of this second lead that can monitor their atrial and sinus node rate. Your cardiologist will make the final recommendation based on your clinical situation. Most pacemakers today allow for additional programming, referred to as “rate-responsive”, that will allow your device to temporarily pace you faster if it detects periods of exercise. This allows for a more natural, physiologic activity of the pacemaker to limit symptoms of fatigue or dizziness that could otherwise arise.
Programming of your pacemaker is a painless and easy procedure. It is accomplished with a “programmer” device that is unique to each manufacturer. A magnetic wand connected to the programmer is placed on top of your skin over your pacemaker allowing for communication of the programmer with your pacemaker generator using radio waves. Newer generation of devices are now allowing wireless communication for ease of use. However, this is limited to several feet, still necessitating an office visit with your physician.
Who needs a pacemaker?
Typically pacemakers are implanted in patients with a history of bradycardia, or slow heart rhythms. These can include the following conditions:
- sick sinus syndrome (sinus node arrest, tachy-brady syndrome, symptomatic sinus bradycardia)
- syncope secondary to a bradycardic rhythm
- atrial fibrillation with a slow ventricular response and bradycardia (due to medications or after AV node junction ablation)
- AV block
- distal conduction system block
- heart failure in patients deemed appropriate for cardiac resynchronization therapy (CRT)
VIDEO: how a permanent pacemaker is implanted
What are the risks?
In general, pacemaker insertion is a safe procedure. However, as with any surgical procedure, there is a risk of complications. The 1-2% risk of complications from permanent pacemaker implantation includes the following:
- bleeding, including a hematoma
- infection
- damage the artery or veins
- blood clot
- tearing the heart muscle
- stroke, death, or heart attack
- puncturing the lung requiring a chest tube
Possible long-term complications you need to be aware of include:
- infection
- pocket erosion
- device or lead malfunction
- lead insulation failure, or lead conductor fracture necessitating the placement of a new lead
The day of the procedure
- Please arrive at the hospital “fasting” from the previous midnight
- You may take your morning medications with a small sip of water
- If you have been instructed to have blood drawn, please do not forget (you may be instructed to have this done several days before your procedure)
- Please make sure you have consulted with your physician if you are on coumadin or insulinfor diabetes. For most procedures, your coumadin will be discontinued or adjusted several days prior.
What to expect after the procedure
- Procedure duration is typically 1-3 hours
- You will have an arm sling for 24 hours
- Overnight hospital stay is generally advised
- You will be instructed to perform daily dry dressing changes at home to the incision site.
- You may be asked to keep the incision site dry for the following week after implantation (you may shower, but need to keep the affected site dry).
- You will need to return to the clinic in 1 week after device implantation
- You can return to normal activities within several days
- Typically driving is discouraged for at least 1 week or longer after the device is implanted
- Extreme motion with the involved arm (above the shoulder) should be avoided for 4-6 weeks after device implantation (this includes activities such as swimming and golf); this could result in lead dislodgement
Usually only a small bump is noticed on the skin. Overtime, most patients do not feel or notice the presence of the device. You will be given an identification card by the device company; it is recommended that you keep this card with you, especially when you travel to the airport or visit a medical provider. Your physician will see you again typically 6 weeks after your pacemaker implantation to examine the incision site and for device programming. Thereafter, expect to follow-up every 3-6 months to monitor the device function and the battery life. Most pacemaker battery’s last 5-8 years, depending on each individual’s degree of pacing.
Precautions
- Be wary of contact sports
- Avoid cellular phone calls directly over your pacemaker generator
- Magnetic resonance imaging (MRI) scans should be avoided unless your physician deems otherwise
- Avoid prolonged exposure in the vicinity to electronic security systems, including metal-detector “wands” and those located at the entrance of most stores
- Avoid working near heavy or high-voltage machinery that can generate magnetic fields
- Avoid exposure to arc-welding equipment





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office