AV Nodal Reentrant Tachycardia (AVNRT)
Overview
AV nodal reentrant tachycardia, AVNRT, is the most common cause of supraventricular tachycardia (SVT). It is more common in women than in men and presents in all age groups. Patients with AVNRT have at least two pathways of tissue in their AV node that allows for an abnormal electrical circuit to perpetuate within their AV node. However, there are many individuals who have dual pathways of AV nodal tissue, but never have the electrical circuit perpetuate to develop sustained tachycardia. It is this spinning circuit that goes “round-and-round” enclosed in the AV node that allows for rapid stimulation of the ventricles through the normal His bundle, bundle branches, and ultimately Purkinje fibers to the ventricular muscle.
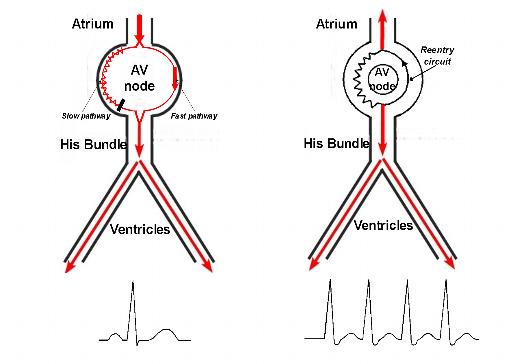
Figure 1. On the left, schema of the AV node during normal sinus rhythm in a patient with two distinct AV nodal pathways, a slow and a fast pathway. The EKG of a normal sinus beat is shown at the bottom. On the right, schema of AVNRT which occurs when an atrial impulse self-perpetuates and revolves in the AV node in a pattern of circuit reentry. These AV nodal reentry beats stimulate both the atrium and the ventricles rapidly in typically a 1 to 1 fashion with a strip of the EKG shown at the bottom.
The symptoms of AVNRT are similar to other SVT, with palpitation, lightheadedness, dizziness, shortness of breath, reduced exercise capacity, weakness, fatigue, chest discomfort, and sweating episodes. These symptoms are primarily due to loss of atrioventricular synchrony (when then atria and ventricles no longer contract in a tightly-coupled progression) or the development of rapid and/or irregular ventricular rates.
Figure 2. Animation of AVNRT with a reentrant circuit revolving around the AV node, leading to rapid stimulation of the ventricle and clinical tachycardia, AVNRT – the most common form of SVT.
Diagnosis
AV nodal reentry tachycardia can be diagnosed by your physician via an electrocardiogram or an Ambulatory monitoring device, i.e. Holter or Event monitor, specifically during an arrhythmia episode. These episodes of SVT can be intermittent and not reliably present on a daily basis. In these situations, your physician may recommend a special ambulatory monitoring device that is patient-triggered, i.e. an Event monitor. Because Ambulatory monitoring devices, such as Holter monitors and Event monitors are only able to record one or two EKG leads, this may make discrimination of AVNRT from other SVT difficult. In addition, the 12-lead of AVNRT can be difficult to differentiate from other SVT including atrial tachycardia and atrioventricular reciprocating tachycardia (AVRT). For patients who require an unequivocal diagnosis, or are candidates for a “curative” catheter ablation procedure, an intracardiac electrophysiology study is the “gold standard” test to establish the diagnosis (see below).
Prognosis
AV nodal reentry tachycardia, as an isolated rhythm disturbance, is not considered a life-threatening condition. Some patients are able to reduce their symptomatic episodes with life-style modification, including avoidance of caffeinated beverages, alcohol, sleep-deprivation, stressful situations, and anxiety. The frequency or severity of symptoms may fluctuate from time-to-time, but they rarely disappear. Because the arrhythmia is due to an abnormal electrical circuit in the heart, there is little any patient can do by himself or herself to prevent or suppress the arrhythmia completely.
Therapy
Therapy for patients suffering from AVNRT depends on the frequency and severity of symptoms. Your physician may decide to implement therapy with oral medications if you are having frequent episodes that affect your daily living. As well, your physician may ask you perform certain “vagal” maneuvers once an episode of AVNRT appears, to help terminate it. The Valsalva maneuver, in which the patient takes a deep breath in, holds it, and then bares down as if they were having a bowel movement, is sometimes effective in terminating AVNRT. Carotid massage, in which the patient presses and rubs on the region of the neck where the carotid pulse is most prominently felt also may be helpful. However, this procedure must be done with care or avoided in the elderly, and in those patients with evidence of occlusive carotid artery disease and bruits (please consult your physician).
 Medications used to terminate symptomatic AVNRT episodes and to reduce AVNRT occurrences include beta-blockers, calcium channel blockers, and less commonly digoxin. These medications can be administered orally on a routine outpatient basis, or via intravenous route if necessary in the emergency room. Some patients may need a combination of medications from different classes. Drug response is variable and highly individualized, with some patients responding and others not. It is a trial and error proposition, with no possibility of knowing what would be most effective for each individual patient ahead of time. Treatment of symptomatic episodes of AVNRT is difficult on an outpatient basis for those patients who do not wish to take a daily regimen of medications. Oral medications take at least a couple of hours to be absorbed, by which time most paroxysms of AVNRT self-terminate, terminate with vagal maneuvers performed by the patient, or are symptomatic enough to prompt an ER visit with IV medications used to terminate the episode. There is no role for antiarrhythmic drug therapy for AVNRT if continued symptomatic breakthrough episodes occur despite lifestyle modifications and oral b-blockers or calcium-channel blockers.
Medications used to terminate symptomatic AVNRT episodes and to reduce AVNRT occurrences include beta-blockers, calcium channel blockers, and less commonly digoxin. These medications can be administered orally on a routine outpatient basis, or via intravenous route if necessary in the emergency room. Some patients may need a combination of medications from different classes. Drug response is variable and highly individualized, with some patients responding and others not. It is a trial and error proposition, with no possibility of knowing what would be most effective for each individual patient ahead of time. Treatment of symptomatic episodes of AVNRT is difficult on an outpatient basis for those patients who do not wish to take a daily regimen of medications. Oral medications take at least a couple of hours to be absorbed, by which time most paroxysms of AVNRT self-terminate, terminate with vagal maneuvers performed by the patient, or are symptomatic enough to prompt an ER visit with IV medications used to terminate the episode. There is no role for antiarrhythmic drug therapy for AVNRT if continued symptomatic breakthrough episodes occur despite lifestyle modifications and oral b-blockers or calcium-channel blockers.
For those patients who elect to forgo medication either due to
- intolerable symptoms or side effects from their medications,
- recurrent symptoms and episodes despite medical therapy, or
- lack of desire to take daily medications for an extended period of time,
your physician may recommend you undergo an electrophysiology study (EPS) and possible “curative” catheter ablation. In brief, these procedures are performed in a special procedure room called an electrophysiology (EP) laboratory. The EP laboratory houses a table and an x-ray (fluoroscopy) machine that is suspended over the table. With the use of specialized electronic and computer equipment, in conjunction with the intracardiac electrode catheters (placed into the heart via the femoral veins), your heart rhythm specialist will use fluoroscopic and electrical guidance to deliver radiofrequency energy to one limb of the perpetuating AVNRT circuit (within the AV node), thus eradicating the rhythm disturbance.
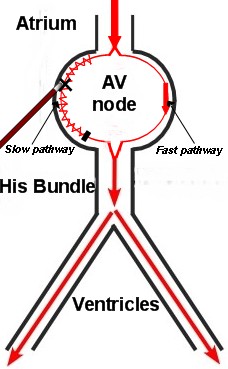
Figure 3. Schema of the AV node with radiofrequency energy delivered via an ablation catheter, typically at the site of the slow pathway to eradicate the circuit that initiates and perpetuates AVNRT.
Radiofrequency energy employed during the catheter ablation procedure heats the tissue enough to destroy the local heart cell function, but without physically cutting through the tissue. The long-term success rate for catheter ablation of AVNRT is well above 90%. However, recovery of tissue function months to years later is possible as the heart attempts to heal itself, with a delayed return of AVNRT. These cases can be approached with a repeat ablation procedure with similarly higher success rates. The risk of serious complication, including complete heart block requiring implantation of a permanent pacemaker, is 1% or less. This complication is an inherent risk of the procedure given the targeted electrical circuit resides within the normal conduction system, i.e. AV node. The risks of radiofrequency catheter ablation for AVNRT are very small and will be discussed in detail with each patient by their heart rhythm specialist at the time of the initial office visit.
In the end, the patients who choose the ablation procedure over no treatment or medical options have decided that the improvement in their quality of life resulting from elimination of the tachycardia (and cure) far outweigh the very small risks associated with undergoing the procedure.





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office