Cardioversion
Why do I need a cardioversion?
 A cardioversion procedure may be performed by your physician to convert you back to normal sinus rhythm if you are suffering from a cardiac arrhythmia. Typically it is done in situations where a patient has a heart rhythm disturbance that has failed medication therapy, such as with antiarrhythmic drugs. Both supraventricular (rhythms that originate from the top 2 chambers of the heart – the atria) and ventricular (rhythms that originate from one of the bottom two ventricles) arrhythmias can be amenable to cardioversion. The most common outpatient arrhythmias that undergo elective outpatient cardioversions are atrial fibrillation and atrial flutter. A more emergent cardioversion is performed on those patients in the hospital or encountered by the EMS team who are suffering from unstable ventricular arrhythmias or atrial fibrillation with very fast and uncontrollable heart rates.
A cardioversion procedure may be performed by your physician to convert you back to normal sinus rhythm if you are suffering from a cardiac arrhythmia. Typically it is done in situations where a patient has a heart rhythm disturbance that has failed medication therapy, such as with antiarrhythmic drugs. Both supraventricular (rhythms that originate from the top 2 chambers of the heart – the atria) and ventricular (rhythms that originate from one of the bottom two ventricles) arrhythmias can be amenable to cardioversion. The most common outpatient arrhythmias that undergo elective outpatient cardioversions are atrial fibrillation and atrial flutter. A more emergent cardioversion is performed on those patients in the hospital or encountered by the EMS team who are suffering from unstable ventricular arrhythmias or atrial fibrillation with very fast and uncontrollable heart rates.
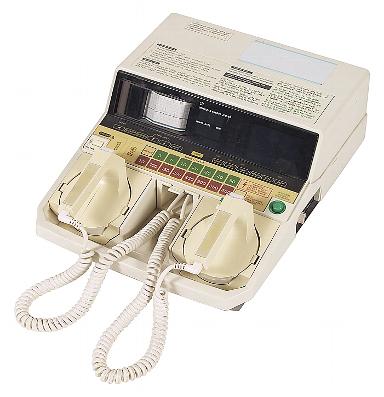
Figure 1. Image of an external defibrillator machine used to perform cardioversions.
The Normal Heart
In brief, as discussed in the Normal Heart section, the sinus node, a structure in the high right atrium, depolarizes typically 60 to 100 times per minute sending an electrical impulse throughout both atria to the AV node. In brief, this leads to synchronized biatrial contraction before ventricular (lower chamber) contraction forces blood out of the heart into the circulation. The AV node, a structure that sits in the middle of the heart, is normally the only electrical connection between the atria and the ventricles. The AV node serves as a traffic signal, controlling the rate of electrical impulses from the atria allowed to reach the ventricles, limiting the danger of 1 to 1 conduction of fast rhythms from the atrium to the ventricles.
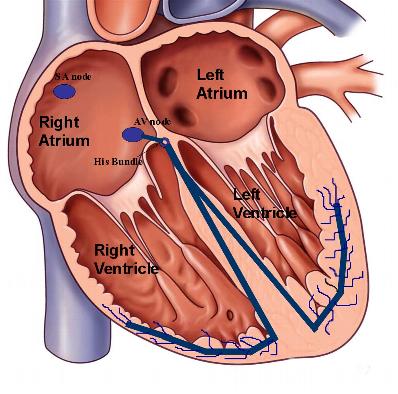
Figure 2. Illustration of the normal conduction system. The sinus node, located in the high right atrium depolarizes and sends an electrical impulse through both atrium typically at a frequency of 60 – 90 beats per minute. In order for this impulse to reach the ventricles in normal hearts, it must traverse the AV node where it encounters a normal minimal delay before it continues its path to the ventricles via the bundle branches.
Atrial Fibrillation
During atrial fibrillation, the atria can contract anywhere from 400-600 beats per minute, in an irregular and chaotic fashion. Fortunately, the AV node, the “traffic control” center, prevents 1 to 1 conduction to the ventricles. It may allow every 2-3 atrial beats to pass to the ventricles in an irregular fashion. The result of the chaotic atrial activity and the fast, irregular response of the ventricles leads typically to symptoms of palpitations, chest fluttering, dizziness, shortness of breath, and possibly fatigue. Depending on your medical history, your physician may therefore recommend you to undergo an elective cardioversion.
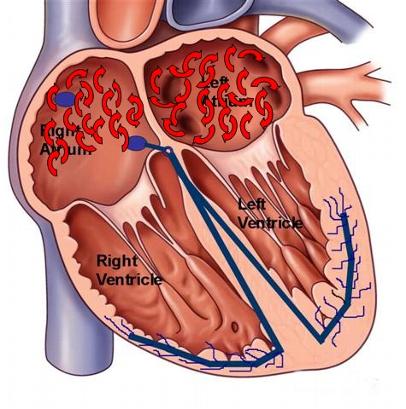
Figure 3. Depiction of atrial fibrillation, with chaotic electrical depolarization of the upper atrial chambers.
What to expect
Typically your physician will ask you to be “fasting” (nothing to eat) starting the midnight before the procedural day. You may take your medications with a sip of water that morning, but consult your physician’s office for specific instructions. You will be brought to a special procedural room where you will be connected to heart and BP monitoring machines. There will be nurses and possibly even anesthesiologists (physicians who specia lize in sedation) present to monitor you and your respirations during the procedure. Two adhesive pads will be placed on your chest, typically one in the front and one on your back to perform the procedure. After placing you to sleep, a small electrical shock, synchronized to your heart’s contractions, will be delivered to the two pads on your chest, capturing the heart’s electrical signal and reverting you back to normal sinus rhythm. This shock attempts to electrically capture all of the heart cells, thus interrupting and terminating the abnormal rhythm disturbance.
lize in sedation) present to monitor you and your respirations during the procedure. Two adhesive pads will be placed on your chest, typically one in the front and one on your back to perform the procedure. After placing you to sleep, a small electrical shock, synchronized to your heart’s contractions, will be delivered to the two pads on your chest, capturing the heart’s electrical signal and reverting you back to normal sinus rhythm. This shock attempts to electrically capture all of the heart cells, thus interrupting and terminating the abnormal rhythm disturbance.
Figure 4. Illustration of an electrical cardioversion procedure.
There is a high success rate of this procedure to converting you back to normal sinus rhythm, but depending on your rhythm disturbance and its duration, sometimes it is not possible to maintain you in normal rhythm; that is, you make convert to normal sinus rhythm, but soon thereafter (even seconds later), revert back to your arrhythmia. This condition is seen more commonly in patients with long-standing atrial fibrillation not on medications. A cardioversion procedure is not appropriate for all patients with atrial fibrillation, and your physician will review your medical history carefully with you. Rarely, you may have some redness at the site of the placement of the chest pads and the electrical shock.
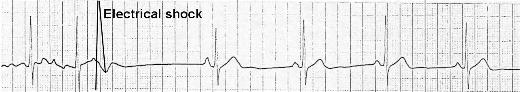
Figure 5. Delivery of electrical cardioversion shock with conversion of atrial fibrillation on the left side of the tracing, to normal sinus rhythm on the right.
Typically you will be able to go home the same day of the procedure after a short recovery phase to allow the sedating medications to wash out. Because you have been given sedation, you will need someone to bring you to the hospital and to drive you home.
Blood Thinners and Anticoagulation
If you have a history of atrial fibrillation and the cardioversion is scheduled to convert you back to normal sinus rhythm, you will generally need to obtain once weekly labs for a total of 4 weeks showing therapeutic blood thinning levels before the cardioversion can be performed. The lab test, an INR (International Normalized Ratio), is a measure of the systemic therapeutic level of your warfarin (a blood thinner, also known as coumadin) medication. Generally, we like to have an INR in the range of 2-3. This is done to reduce the risk of suffering a stroke if you have a clot in the left atrium. Anticoagulation (blood thinners) helps to prevent the formation of clots in the top atria that occur during atrial fibrillation due to the stasis of blood that occurs when the atria are chaotically beating 400-600 beats per minute. With a cardioversion procedure, there is a risk of dislodging any clots in the heart upon restoration of normal sinus rhythm and atrial synchronized contraction. Some patients may elect to forgo the anticoagulation therapy before cardioversion by consenting for a procedure called a transesophageal echocardiogram (TEE). A TEE is an ultrasound that allows visualization of the left atrium to rule out a “silent” clot in the heart. It is performed by placing a small ultrasound probe under sedation into the esophagus to better visualize the heart chambers. This procedure is relatively short, typically lasting less than 15 minutes. If there is no clot, your physician will proceed with the cardioversion. After the cardioversion, you will need to be on anticoagulation for at least 4 weeks, if not longer, depending on your medical history. This is to prevent the formation of a clot that can occur with “stunning” of the atria immediately after cardioversion. If you have had atrial fibrillation that is proven to be less than 48 hours, your physician may elect to cardiovert you immediately, as the risk of clot formation in the heart is significantly low in this time frame that you do not need pre-procedural anticoagulation.
Instead of an electrical cardioversion, your physician may opt to perform a chemical cardioversion. A chemical cardioversion is administered via antiarrhythmic medications typically through an intravenous route (can be done as an outpatient with oral medications as well). The procedural preparation would be the same, with continuous electrical and respiratory monitoring after injection of the agent. These medications typically take longer to convert a patient to normal sinus rhythm, and if unsuccessful, your physician may opt to electrically cardiovert you the same day. Your physician will discuss the risks and benefits of both scenarios, including the small incidence of pro-arrhythmias with the use of intravenous antiarrhythmic medications.
How to prepare
- Remember to be fasting starting the midnight before the procedure
- Take your medications that morning with a sip of water
- Have a dedicated driver escort you to the hospital and back home after the procedure due to issues with sedation and driving
- Consult your physician to ensure you have the adequate laboratory documentation of weekly INR values for the 4 weeks prior to your procedure
- Local skin irritation and transient redness from the electrical shock can be experienced.





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office