Cardiac resynchronization therapy (CRT)
What is a CRT device?
Cardiac resynchronization therapy (CRT), also known as biventricular pacing, is an electrical method to coordinate and synchronize your heart’s contraction in an attempt to improve your symptoms of heart failure. Not everyone with heart failure is a candidate for CRT. Your physician will screen you based on tests including your ejection fraction and your 12-lead EKG. As well, you must have persistent heart failure despite maximal medication therapy.
As discussed in the previous “Your Heart” section, the heart has its own pacemaker comprised of specialized conduction cells in the top right atrium, known as the sinus node. The sinus nodetypically fires at a rate of 60–90 times per minute. This electrical depolarization wave leads to the contraction of the upper atria with the signal traversing the AV node, located in the center of the heart in between the upper and lower chambers, to the ventricles with synchronized ventricular contraction. In heart failure, this synchronized control of the pumping of the lower chambers can be disrupted, with a resultant delay in either left or right ventricular contraction. A representative 12-lead EKG finding of this contraction delay is the presence of left bundle branch block (LBBB). Left bundle branch block (seen as a widened QRS complex) suggests left ventricular contraction delay, with the right ventricular beginning contraction first. This resultant asynchronous and uncoordinated ventricular contraction can worsen heart failure or be the result of heart failure.
Biventricular pacing can be performed as either a biventricular pacemaker alone or a bundled device, a biventricular ICD. The primary difference is that the biventricular ICD has a generator that can perform defibrillation via the specialized right ventricular shocking coil lead. As with previously discussed pacemakers and ICD systems, an atrial lead can also be implanted if necessary.
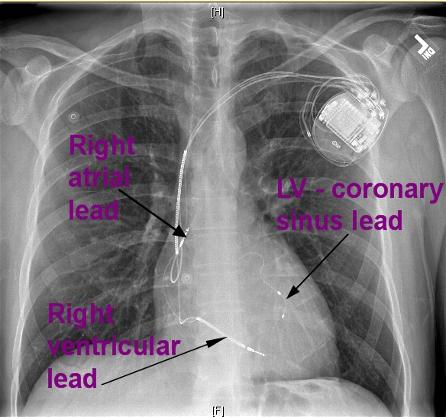
Figure 1. Chest X-ray of a CRT device in the chest.
A CRT device has a left ventricular pacemaker lead, also known as a “coronary sinus” lead. This lead is also implanted via the central veins of the chest. Under X-ray guidance, this specialized left ventricular pacing lead is placed into a structure known as the “coronary sinus“. This structure is located in the right atrium and drains the blood supply of the heart. Consequently, the vein courses along the back side of the heart to the left ventricular wall. By accessing this vein, the left coronary sinus lead can be positioned along the left ventricular wall to provide selective pacing of the left ventricle that can be coordinated with the right ventricle via the right ventricular pacing lead . This resultant coordinated biventricular pacing can reduce the right and left ventricular electrical delay and improve cardiac function and symptoms of heart failure.
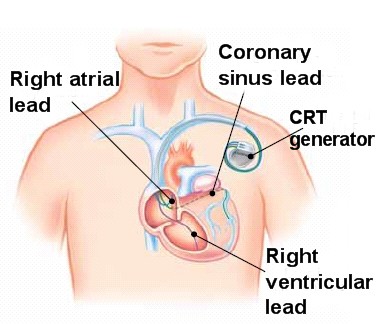
Figure 2. Illustration of a CRT device in the chest, with a left ventricular lead placed via the coronary sinus under X-ray guidance.
When is CRT the right choice?
Patients who qualify for CRT implant are based on studies done in particular subgroups of patients. They typically must satisfy the following:
- Depressed left ventricular ejection fraction < 35%
- Evidence of asynchronous, uncoordinated left and right ventricular contraction with left bundle branch block (LBBB) on 12-lead EKG
- Moderate to severe symptoms of heart failure, despite lifestyle changes and maximal medications

Figure 3. Panel A shows an EKG strip of LBBB in a patient with heart failure and dysynchronous ventricular contraction. With implantation of a CRT system, the patient’s biventricular-paced EKG in Panel B shows narrowing of the QRS-complex with synchronous ventricular contraction.
About two-thirds of patients who undergo CRT implantation report improvement in their symptoms of heart failure. This can be immediate or take weeks as the cardiac muscle remodels. However, still a significant portion of those implanted, that is at least one-third, do not respond to biventricular pacing. Medical management and lifestyle modification is paramount and first-line therapy for congestive heart failure patients.





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office