Implantable cardioverter defibrillator (ICD)
What is an ICD?
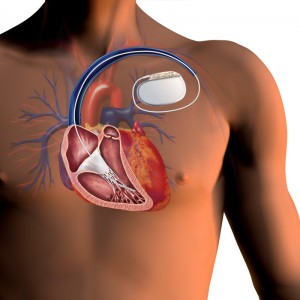
An ICD is an implantable battery-operated device (the “generator”), about the size of a pager, packed full of electrical circuitry with the sole function to monitor your heart’s own rhythm and to deliver a life-saving high-energy electrical defibrillation shock if a dangerous ventricular tachyarrhythmia is detected. The ICD system consists of the generator (typically referred to as the “ICD”) and at least one lead, typically a right ventricular defibrillation lead.

Figure 1. Image of a typical ICD generator beside a pacemaker generator.
As discussed in the previous sections, your normal heart has its own pacemaker comprised of specialized conduction cells in the top right atrium, known as the sinus node. The sinus nodetypically fires at a rate of 60–90 times per minute. This electrical depolarization wave leads to the contraction of the upper atria with the signal traversing the AV node, located in the center of the heart in between the upper and lower chambers, to the ventricles with synchronized ventricular contraction. An arrhythmia, or heart rhythm disturbance, can develop in any of the cardiac chambers. Ventricular tachyarrhythmias are generally the most dangerous, as they result in fast heart rates and hemodynamic collapse.

Figure 2. Illustration of ventricular tachycardia and fibrillation originating from the ventricular muscle tissue. An EKG strip of ventricular fibrillation as a result of this chaotic ventricular electrical activity.
All modern ICD systems can also function as pacemakers, being able to conduct an electrical pacing impulse from the generator to the tip of the leads and the heart. The ICD lead is more complex than your average pacemaker lead. These insulated wires have both pacing and defibrillation functions. As a result, they tend to be thicker than your average pacemaker lead, with an externally visualized “shocking coil” along the body. This shocking coil allows for the internal defibrillation of the heart with a high-energy current delivery from the generator if ventricular tachycardia is detected. These shocks can be painful and are likened to being kicked in the chest.
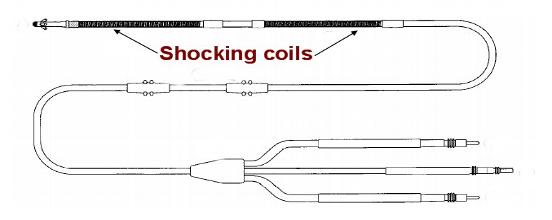
Figure 3. Schema of a typical ICD lead. The distal electrode tip in contact with the heart has typically two shocking coils that allow for a high-energy discharge to be delivered to the heart to defibrillate a patient with ventricular tachycardia or fibrillation.
The ICD leads are implanted via the central chest veins and using fluoroscopic, or X-ray, guidance they are maneuvered into position into the right-sided heart chambers.
Figure 4. Schema of an ICD implant with the generator typically placed in the left chest just underneath the skin. The ICD leads are placed into the heart via the central veins and typically screwed into position in the right ventricle.
The opposite-end of the intracardiac lead is then screwed into the ICD generator. Once implanted, these leads can sense your own heart’s electrical signals and if too slow, pace accordingly. A small painless electrical current created by the ICD generator flows from the generator through the insulated intracardiac leads to the interface between the lead tip and the heart muscle tissue. Not only is the ICD programmed to pace your heart if it falls below a lower programmable rate, but more importantly, it is capable of delivering an electrical defibrillation shock if your heart rate is too fast and you are suffering from ventricular tachycardia or fibrillation.
As with pacemaker systems, there are “single” and “dual-chamber” ICD systems. Single-chamber systems always refer to presence of one right ventricular ICD shocking coil lead; a dual-chamber system refers to the addition of a right atrial pacemaker lead that can sense the atrial electrical activity. For those patients with a history of sick-sinus syndrome or bradycardia originating from the atria (top chambers of the heart), they typically benefit from implantation of this second lead that can monitor their atrial and sinus node rate. Your cardiologist will make the final recommendation based on your clinical situation.
Programming of your ICD system is a painless and easy procedure. It is accomplished with a “programmer” device that is unique to each manufacturer. A magnetic “wand” connected to the programmer is placed on top of your skin over your device allowing for communication of the programmer with your generator using radio waves. Newer generation of devices are now allowing wireless communication for ease of use. However, this is limited to several feet, still necessitating an office visit with your physician.
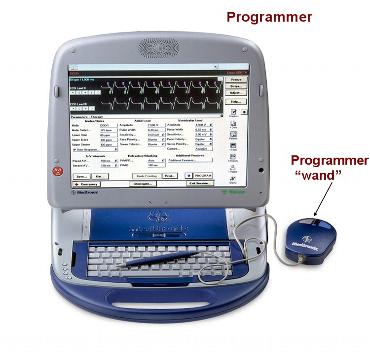
Figure 5. Image of one device manufacturers “programmer”. During office visits, the programmer “wand”is placed over your device and uses radio waves to collect stored data and to check the integrity and functioning of your device and its intracardiac leads.
Who needs an ICD?
ICDs are implanted in the following conditions:
- Survivors of sudden cardiac death
- Primary prevention with a history of structural heart disease and EF<35%
- Primary prevention with a history of structural heart disease and positive electrophysiology (EP) study for ventricular tachyarrhythmia
- Recurrent ventricular tachycardia associated with a history of coronary artery disease or cardiomyopathy
- Recurrent ventricular tachycardia or syncope secondary to an inherited cardiomyopathy or ion channel disease including but not limited to hypertrophic cardiomyopathy, long-QT syndrome, Brugada Syndrome, and Arrhythmogenic right ventricular dysplasia
ICD systems have been proven to prolong survival in a select population. They are the most effective method to reduce the risk of sudden cardiac death in patients with ventricular tachycardia and/or fibrillation or structural heart disease already on medical therapy. The role of antiarrhythmic medication to suppress ventricular tachyarrhythmias in this population as a primary treatment regimen is limited, given it has no survival benefit. However, antiarrhythmics are useful to reduce the burden of ventricular tachyarrhythmias in patients with recurrent ICD shocks. ICDs are not always necessary for patients with ventricular tachycardia and a reversible or treatable cause, including a myocardial infarction, coronary blockage, or medications. Also, ICDs may not be appropriate when other coexisting severe medical conditions that are expected to limit the patient’s life expectancy, including metastatic cancer or severe infection are present.
VIDEO: How to implantable a cardiac defibrillator.
What are the risks?
In general, an ICD insertion is a safe procedure. However, as with any surgical procedure there is a risk of complications. There is a 1-2% risk of complications including:
- bleeding, including a hematoma
- infection
- damage the artery or veins
- blood clot
- tearing the heart muscle
- stroke, death, or heart attack
- puncturing the lung requiring a chest tube
Possible long-term complications you need to be aware of include:
- infection
- pocket erosion
- device or lead malfunction
- lead insulation failure, or lead conductor fracture necessitating the placement of a new lead
The day of the procedure
- Please arrive at the hospital “fasting” (nothing to eat) from the previous midnight
- You may take your morning medications with a small sip of water
- If you have been instructed to have blood drawn, please do not forget (you may be instructed to have this done several days before your procedure)
- Please make sure you have consulted with your physician if you are on coumadin or insulinfor diabetes. For most procedures, your coumadin will be discontinued or adjusted several days prior.
What to expect after the procedure
- Procedure duration is typically 1-3 hours
- You will have an arm sling for 24 hours
- Overnight hospital stay is generally advised
- You will be instructed to perform daily “dry dressing” changes at home to the incision site.
- You may be asked to keep the incision site dry for the week following implantation (you may shower, but need to keep the affected site dry).
- You will need to return to the clinic in 1 week after device implantation for wound check
- You can return to normal activities within several days
- Typically driving is discouraged for at least 1 week or longer after the device is implanted
- Extreme motion with the involved arm (above the shoulder) should be avoided for 4-6 weeks after device implantation (this includes activities such as swimming and golf); this could result in lead dislodgement .
You will be given an identification card by your device company; it is recommended that you keep this card with you, especially when you travel to the airport or visit a medical provider. Your physician will see you again typically 6 weeks after your ICD implantation to examine the incision site and to confirm device programming. Thereafter, expect to follow-up every 3-4 months to monitor the device function and the battery life. Most ICD batteries last 3-6 years.
How to deal with a shock
An ICD defibrillation therapy, or “shock”, can be a frightening and anxiety provoking event. During the first year after implantation the chances of receiving at least one ICD shock ranges from 30-50%. These shocks have been likened to being “kicked” in the chest. Some patient’s experience psychological symptoms, especially after an event that triggers multiple ICD “discharges” in a short period of time. These symptoms range from anxiety to depression, with some patients experiencing “phantom” (perceived, but not real) shocks afterwards.
You may be startled and anxious after receiving an ICD shock, but this should be tempered by the knowledge that your ICD has done its job to protect you from life-threatening tachyarrhythmias.Local support groups are available for patients with ICDs and a history of therapeutic shocks. You should always have your device implantation card available, along with a plan of action if you were to receive a shock. This plan can be discussed with you and your physician, to limit your anxiety at the time of shock. It may be as simple as calling your physician to discuss the event and arrange a time for appropriate follow-up. A single ICD shock is generally not an emergency to prompt a 911 call, but more than 2 in a short time frame is and should prompt you to seek immediate medical attention.
When you see your physician in follow-up, he/she will “interrogate” your device to review the device data regarding the episode of ICD shock. Inappropriate shocks can occur. An inappropriate shock can be secondary to a fast supraventricular tachycardia, a fractured lead or insulation material, or sensing of noncardiac signals by the lead and system (noise). The device, as you can imagine, is programmed conservatively to err on the safe side and deliver a shock in clinical scenarios that may be unclear or during tachycardias that are sustained for prolonged periods, despite not being ventricular in origin. Your physician will discuss the situation with you if this occurs and either reprogram the device or institute additional medical therapy.
Precautions
- Be wary of contact sports
- Avoid cellular phone calls directly over your ICD generator
- Magnetic resonance imaging (MRI) scans should be avoided unless your physician deems otherwise
- Avoid prolonged exposure in the vicinity to electronic security systems, including metal-detector “wands” and those located at the entrance of most stores
- Avoid working near heavy or high-voltage machinery that can generate magnetic fields
- Avoid exposure to arc welding equipment
Magnetic fields can disable the functioning of your ICD and blind it to sensing a ventricular tachyarrhythmia. Conversely, electromagnetic interference (EMI) from security systems and heavy machinery can lead to oversensing of fictitious intracardiac signals leading to inappropriate shocks.https://vimeo.com/178548249





 Silver Spring Office
Silver Spring Office  DC Office (at Providence Hospital)
DC Office (at Providence Hospital)  Hagerstown Office
Hagerstown Office